There is only one absolute in atherosclerosis: sterols (predominantly cholesterol) entering the artery wall and being internalized by macrophages, creating foam cells (the histologic diagnostic marker of atherosclerosis) and the associated inflammatory process. If one can keep sterols out of the intimal layer there cannot be atherosclerosis. – Thomas Dayspring, MD, FACP, Understanding the Entire Lipid Profile
September is National Cholesterol Awareness Education Month, and as an Advocate for Awareness for the Family Heart Foundation, it’s a perfect time to dive into a topic that’s close to my heart.
In Closer to the Heart – Part 1 (April 22, 2023), I discuss the importance of finding root causes of inflammation, its ties to insulin resistance, weight gain, the symptoms of metabolic syndrome, and how it can lead to atherosclerosis. I also shared the physician’s brochure and guide to the Quest CardioIQ tests. The advanced lipid panel tests go beyond conventional lipid panels ordered by most PCPs in that they reveal the particle counts for important markers of cholesterol – the ApoB and Lipoprotein(a) among other. The particle counts are critical information in order to understand your risks.
Let’s go deeper into the heart of the matter to learn what you need to know about your cholesterol and your risks for cardiovascular disease and stroke. Cholesterol is a waxy, fat-like substance found in all the cells of your body. Your body produces the cholesterol it needs to make hormones, Vitamin D, and substances that help you metabolize food. The cholesterol in your blood is mainly synthesized in the liver or reabsorbed from the small intestine. (Foods, such as eggs, cheese, and meat, are dietary sources of cholesterol.)
- High cholesterol is a major risk factor for heart disease, which is the leading cause of death in the United States.
- People with high cholesterol are twice as likely to have heart disease than people with lower cholesterol levels.
- 73.5 million American adults (31.7%) have high low-density lipoprotein (LDL) cholesterol.
- Fewer than 1 out of every 3 adults with high LDL cholesterol has the condition under control.
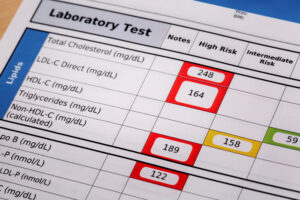
During my weight transformation, at the point when I had lost 70 pounds, I expected my labs would be in normal ranges. And for the most part, they were except my LDL-C was in a high-risk range. Optimal is considered less than <100 and high risk is considered greater than 129 mg/dL.
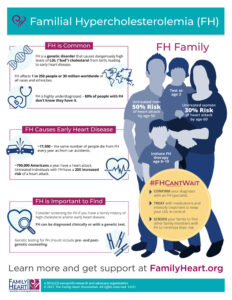
LDL greater than >190 in adults or >160 mg/dL in children may signify that a person has Familial Hypercholesterolemia (FH), an inherited condition characterized by very high levels of cholesterol in the blood. This disorder affects 1 in 250 people and increases the risk of having a heart attack.
A family history of early heart attacks may indicate FH, and it is only necessary to inherit the gene from one parent, but it is possible to inherit from both. Sixty to eighty percent of people with FH have a mutation in the LDLR, APOB, and PCSK9 genes. These are the genes which determine how your body produces and removes cholesterol. Genetic testing is available to check for mutations.
According to the CDC, people with FH often exhibit signs of extra cholesterol built up in different parts of the body:
- Bumps or lumps around the knees, knuckles, or elbows.
- Swollen or painful Achilles tendon
- Yellowish areas around the eyes
- A whitish gray color in the shape of a half-moon on the outside of the cornea
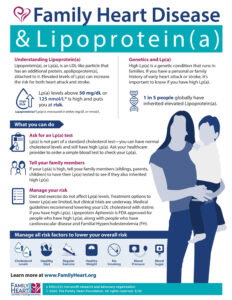
Another genetic condition can be discovered by testing the particle count of Lipoprotein(a), often abbreviated as Lp(a). Elevated Lp(a) is found in 1 in 5 people. Twenty percent of the global human population are born with this marker, which is an independent and triple threat for coronary vascular disease (including aortic stenosis, myocardial infarction and ischemic stroke) in that it increases atherosclerosis, inflammation, and blood clotting. Few doctors are aware if their patients have elevated Lp(a) because it is not part of the standard lipid panel tests; thus, less than one percent of Americans have been tested for it. The European Society of Cardiology recommends that all people are tested for Lp(a) at least once in their lifetime.
If your Lp(a) level is greater than >125 nmol/L (50 mg/dL), you have elevated Lp(a). The Lp(a) particle count reaches its level by the age of 5 and remains stable through most of adult life.
Both of these genetic conditions can be inherited by first degree relatives; therefore, it is important that family members are identified and tested through cascade screening. It’s important to test both adults and children for Lp(a) and FH, because the sooner treatment is begun, the sooner the risk of disease can be mitigated. Testing is often recommended for children as young as age 5, or as young as age 2 if homozygous FH, inherited from both parents, is suspected.
While it is not within my scope of practice as a health coach to diagnose or prescribe, or suggest medications or other treatment, I feel that it is important to share sources of relevant information and prepare clients to speak with their doctors about cholesterol particle testing in addition to their standard lipid panel, and to insist on being tested. Speaking from experience, I had no idea why my LDL-C was high until I took the Quest CardioIQ test, which revealed that I had elevated Lp(a).
You might hear your primary care doctor say that he or she does not know what to do with the data from the advanced lipid panel tests. While treatments for FH and Lp(a) may be in the pipeline, cardiologists often recommend medications to reduce the LDL-C. There are additional nuanced tests that point the way to specific treatments, including the Cholesterol Balance Test, which can determine if you are a hyper-synthesizer or hyper-absorber of cholesterol, or both. Different medications or a combination of medications can be prescribed. If you or your doctor cannot order the Boston Heart Labs tests, you can order an at-home test from empowerDX.
If you have high LDL-C, you should make every effort to know why so that you can obtain the best treatment. The bottom line is this: if we don’t know what’s going on in our own bodies, how can we obtain the best treatment or be ready when the next best treatment comes along?
Shining a light on LDL cholesterol management in America, Dr. Seth Baum discusses treatment and challenges of navigating the healthcare system with the Family Heart Foundation.
♥ Susan L. Ward
Integrative Nutrition Health Coach